Pelvic Organ Prolapse
This is a subtitle for your new post
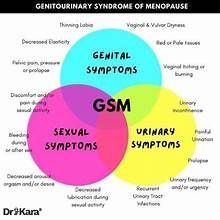
Pelvic organ prolapse (POP). The all too familiar sensation for women that their bladder or uterus is “falling out” of their bodies. That heavy, bulging sensation in the pelvis that’s often accompanied by abdominal pain, urinary incontinence, and an overall feeling of pressure and bother. What is this all about?! What causes it, what are the risk factors, and how can you avoid it?
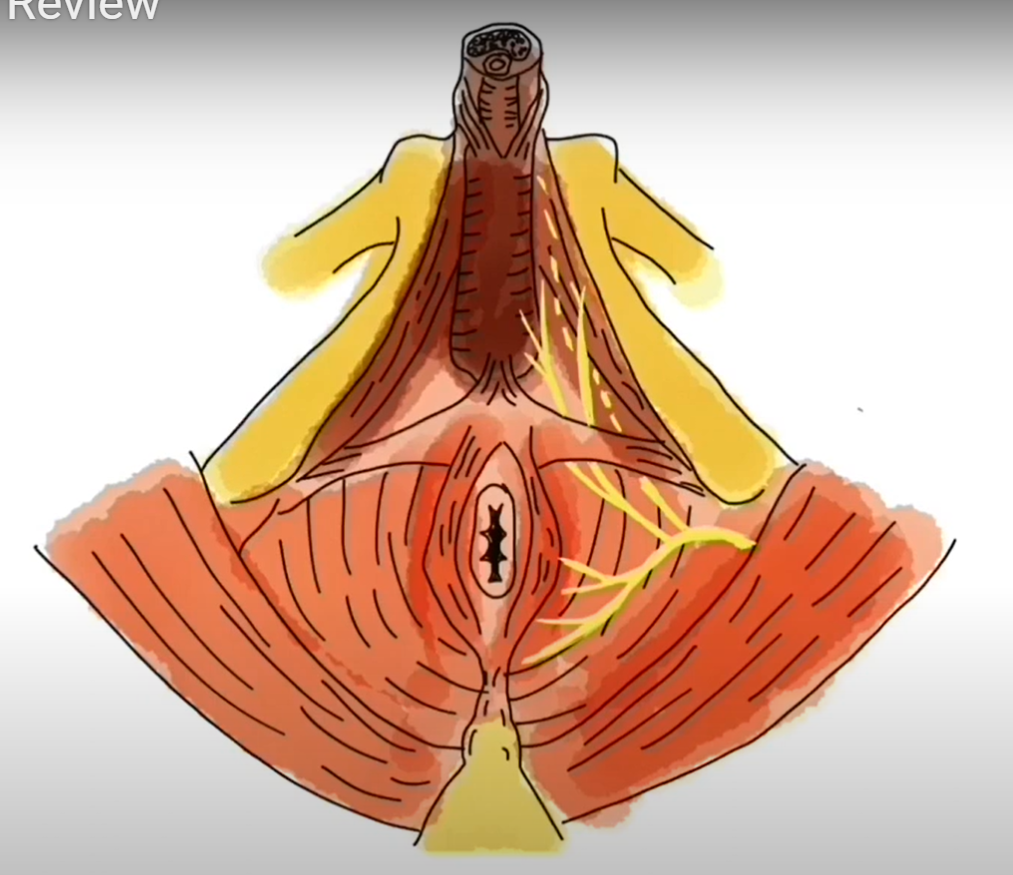
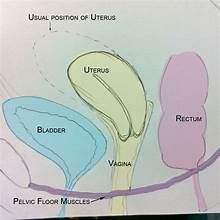
As a PT my first educational point is always anatomy. We can’t fully understand abnormal if we don’t have an idea of normal, right? In the picture below, the top image is a woman’s pelvis showing all the organs in the correct place; the bladder is situated directly behind the pubic bone and in front of the uterus, and the rectum is in its’ place behind the uterus. All of these organs are supported above by ligaments and fascial connections, and below by your pelvic floor muscles (neither are pictured here). In the three images below, you can see examples of the three types of POP:
cystocele (prolapse of the bladder),
rectocele
(prolapse of the rectum), and
apical prolapse
(prolapse of the uterus).
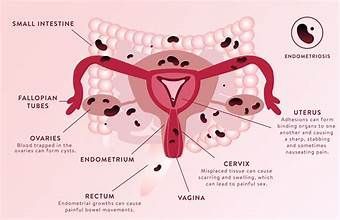
POP is defined as the descent of one or more of the pelvic structures (bladder, uterus, rectum, or vagina) from the normal anatomic location or through the vaginal opening. What causes this descent, or drop, of the pelvic organs? POP is often associated with pregnancy and vaginal deliveries due to the immense stretch the pelvic floor muscles go through during pregnancy and the increase in intra-abdominal pressure that is created with pushing during delivery. Your risk for POP is higher if your child is delivered vaginally, but women who have a Cesarean section are still at risk. Hysterectomy, pelvic surgery, obesity, chronic cough or constipation, and/or repeated heavy lifting are also a few known risk factors for POP (1, 2). When we have an increase in pressure through our abdomen, this puts stress on the ligaments that help to support our pelvic organs. As time passes and we continue to put that pressure on the organs, the ligaments can become stretched and lose the ability to hold the organs in place. As a result, you can have the feeling that something is “falling out,” that something just isn’t right within the pelvis. You might even be able to see something coming out of the vagina that makes it uncomfortable to walk, stand, or exercise.
Because prolapse can involve any or all of the pelvic organs, women with POP may have any of the following bladder, bowel, and/or sexual complaints:
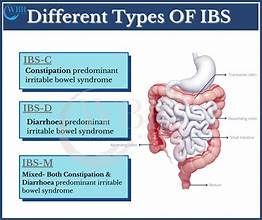
- Inability to fully empty the bowel or the bladder - Ever go to the bathroom, void your bladder, and 20 minutes later feel like you could go again? This could be due to the fallen position of your bladder, making it difficult for you to fully empty.
- Urinary and/or fecal leakage - If your bladder or rectum is not in the correct place, it can be difficult to fully empty. When there is residual stool or urine present, it can leak out during laughing, coughing, sneezing, or exercise. We often see a connection between POP and weak PFM, and when our PFM are weak we can have leakage.
- Discomfort with intercourse - in cases of POP, women have tissue descended down through the vaginal canal that is not supposed to be there. This tissue can cause an increase in pressure, discomfort, or even pain with intercourse.
- Pain or pressure in the low back and abdomen - patients with POP often describe a heaviness, pressure, and general discomfort in the abdomen. When your pelvic organs are descended further than they should be, this puts pressure on the areas to which the organs attach - your abdominal wall and the bones of your lower spine/sacral area.
So, what can be done for this?
Pelvic health physical therapy for POP targets a few things:
- First, we work on strengthening the pelvic floor muscles. Since these muscles are located at the bottom of your pelvis, just underneath all of these internal organs, they serve as a big support system for your bladder, uterus, and rectum. If the ligaments that help to maintain stability are loose, it’s even more important that the pelvic floor muscles are strong enough to provide dynamic support throughout your day. Often times women have been experiencing symptoms of bulging or heaviness in the pelvis for awhile and their pelvic floor muscles have been working overtime to support the prolapse, resulting in a pelvic floor that is overactive or too tight. In this case, we would focus on teaching you to relax your muscles, and then move on to strengthening. Not sure if your muscles are too tight or too loose? See a pelvic health PT!
- Another big component of prolapse management is core stabilization and control of intra-abdominal pressure (IAP). The majority of risk factors for POP involve some sort of increase in the pressure throughout your abdomen and pelvis: pregnancy, delivery, increased weight, heavy weight lifting, chronic cough or straining with bowel movements, etc. We will naturally do things throughout our day that increase this pressure, but if our deep core muscles are not coordinated and strong enough to equally distribute that pressure, it can be directed straight down onto the pelvic organs and make the prolapse worse. For full understanding of this, sit up straight in your chair, close your mouth, and push down into your pelvis as if you’re trying to have a bowel movement or deliver a baby vaginally. Can you feel all of that pressure going straight downwards? That is what we want to avoid, specifically for women with prolapse but for all women! This kind of pressure is not beneficial for your pelvic floor, abdomen, or pelvis. In the picture below, you can see the four muscles of our “deep core.” Each of these muscles will be strengthened with therapy so they are able to evenly distribute that IAP throughout your day. See references at the end of the post for more details about your core and how to manage it (4).
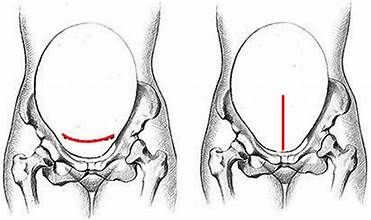
- Posture is also an important component of care. The ideal position of your core involves getting your rib cage “stacked” on top of your pelvis, without too much curve or flattening of your lower back. When the bones of our pelvis and spine are aligned just right, the muscles that attach to them (our deep core muscles) are able to function at their very best.
If you’re curious about whether or not you’re experiencing symptoms of POP, see the questionnaire below for more detailed questions (3). Pelvic floor PT is a great first step if you’re experiencing any symptoms of pelvic organ prolapse, as it carries very few risks. If you finish your therapy and are still having symptoms, there are interventions from other members of your medical team that can be beneficial, including pessary placement or surgery. Always feel free to talk to your medical provider about the symptoms you are having and the options available!
- Iglesia CB1, Smithling KR. Pelvic Organ Prolapse. Am Fam Physician. 2017 Aug 1;96(3):179-185.
- Gyhagen M, Bullarbo M, Nielsen T, Milsom I. Prevalence and risk factors for pelvic organ prolapse 20 years after childbirth: a national cohort study in singleton primipara after vaginal or cesarean delivery. BJOG 2012; DOI : 10.1111/1471-0528.12020.
- Pelvic Floor Distress Inventory. https://legacybhsapps.beaumont.edu/Global/Urology/WUC_Pelvic_Floor_Questionnaire.PDF/
4. Julie Wiebe, PT. Dear Coach. http://www.juliewiebept.com/alignment/dear-coach/